Medical drainage systems play a crucial role in patient care, particularly for individuals requiring continuous bladder drainage. A urine bag serves as an essential medical device designed to collect and contain urine safely while maintaining optimal hygiene standards. These specialized collection systems have revolutionized patient comfort and clinical efficiency in healthcare settings worldwide.
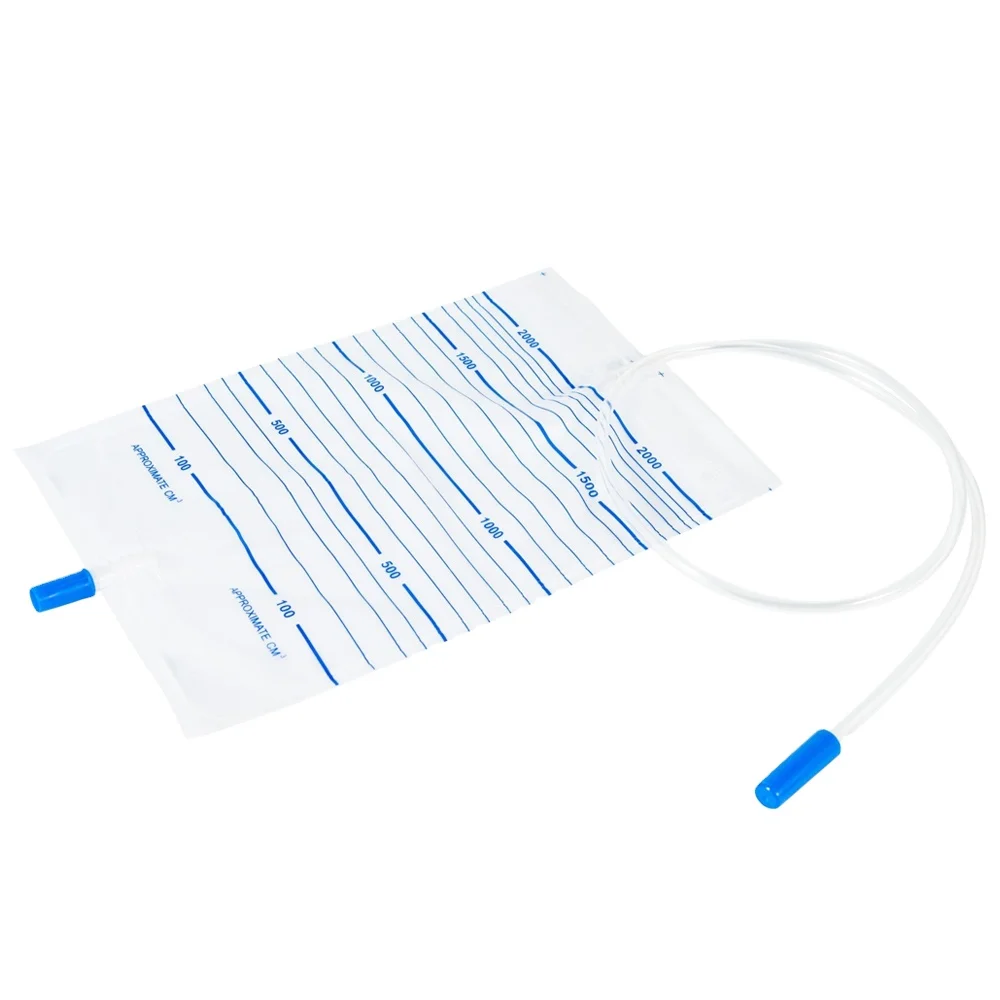
Healthcare professionals depend on reliable drainage solutions that prevent contamination and ensure patient dignity. Modern urine bag technology incorporates advanced materials and engineering principles to deliver superior performance in clinical environments. Understanding how these devices function helps medical staff provide better patient care while reducing infection risks.
The design complexity of contemporary drainage bags reflects decades of medical innovation focused on improving patient outcomes. Each component serves specific functions that contribute to overall system effectiveness and safety. This comprehensive analysis explores the mechanisms that make urine bag systems reliable for long-term medical use.
Advanced Design Features of Modern Urine Bags
Multi-Layer Construction Technology
Contemporary urine bag manufacturing employs sophisticated multi-layer construction techniques that enhance durability and prevent leakage. The outer layer typically consists of medical-grade polyethylene or similar materials that resist punctures and chemical degradation. This protective barrier shields the inner collection chamber from external contamination while maintaining structural integrity under varying pressure conditions.
The inner layer of a quality urine bag features specialized coatings that prevent bacterial adhesion and biofilm formation. These antimicrobial surfaces reduce infection risks by inhibiting pathogen growth within the collection system. Advanced manufacturing processes ensure uniform coating distribution across all internal surfaces, creating consistent protection throughout the device lifespan.
Between the outer and inner layers, manufacturers often incorporate barrier films that provide additional leak protection. These intermediate layers serve as backup containment systems, ensuring that even if the primary collection chamber experiences minor damage, fluid remains contained within the device structure.
Precision Valve Mechanisms
The valve system represents the most critical component of any urine bag, controlling fluid flow and preventing backflow contamination. Modern valves incorporate spring-loaded mechanisms that automatically seal when drainage pressure decreases. This automatic closure prevents retrograde flow that could introduce bacteria into the bladder or catheter system.
High-quality valve assemblies feature multiple sealing surfaces that create redundant barriers against leakage. These precision-engineered components undergo rigorous testing to ensure consistent performance across thousands of opening and closing cycles. The materials used in valve construction resist degradation from exposure to urine and cleaning solutions.
Some advanced urine bag models incorporate pressure-sensitive valves that adjust opening force based on fluid volume. This adaptive functionality prevents excessive pressure buildup while maintaining secure closure during normal operation. Such innovations demonstrate the ongoing evolution of drainage bag technology toward improved patient safety and comfort.
Hygiene Maintenance Through Sterile Design
Sterile Manufacturing Processes
Manufacturing facilities producing medical-grade drainage bags operate under strict sterile conditions that exceed standard industrial cleanliness requirements. Every stage of urine bag production occurs within controlled environments where air filtration, humidity, and temperature parameters remain constant. These conditions prevent contamination during assembly and packaging processes.
Gamma radiation sterilization represents the gold standard for medical device sterilization, effectively eliminating all microorganisms without compromising material properties. Each urine bag undergoes this treatment before packaging, ensuring complete sterility upon opening. Quality control testing verifies sterility levels meet international medical device standards.
Packaging systems for sterile drainage bags incorporate multiple barrier layers that maintain sterility during storage and transportation. These protective packages include tamper-evident seals and expiration date labeling to ensure proper inventory management in healthcare facilities.
Antimicrobial Surface Treatments
Advanced urine bag designs incorporate antimicrobial surface treatments that actively inhibit bacterial growth throughout the device lifespan. Silver ion technology represents one popular approach, where microscopic silver particles embedded in bag materials continuously release antimicrobial agents. These treatments significantly reduce infection rates associated with long-term drainage bag use.
Copper-based antimicrobial coatings offer another effective approach to maintaining hygiene within drainage systems. These treatments work by disrupting bacterial cell walls upon contact, preventing colonization of bag surfaces. Research demonstrates that copper-treated surfaces remain effective against pathogens for extended periods without requiring replacement.
Some manufacturers employ photocatalytic surface treatments that generate reactive oxygen species when exposed to ambient light. These self-cleaning surfaces continuously break down organic contaminants and bacterial biofilms, maintaining cleaner internal environments within the urine bag throughout its use period.
Leak Prevention Engineering Solutions
Pressure Distribution Systems
Effective leak prevention in drainage bags requires careful attention to pressure distribution across all connection points and seams. Engineers design urine bag systems with reinforced stress points that handle varying fluid pressures without compromising seal integrity. These reinforcements typically involve thicker materials or additional bonding layers at critical junction areas.
Flexible mounting systems allow drainage bags to move with patient activity while maintaining secure connections to catheters and bed rails. These mounting mechanisms distribute mechanical stress across multiple attachment points, preventing concentrated forces that could cause connection failures or bag damage.
Advanced pressure relief systems automatically vent excess pressure that could otherwise cause bag rupture or connection failure. These safety mechanisms protect both the urine bag integrity and patient comfort by preventing excessive pressure buildup during periods of high fluid output.
Connection Interface Optimization
The interface between catheters and drainage bags represents a critical point for potential leakage and contamination. Modern connection systems employ standardized fittings that ensure secure, leak-proof attachments while allowing for easy disconnection when necessary. These standardized interfaces reduce compatibility issues and improve overall system reliability.
Luer-lock mechanisms provide secure threaded connections that resist accidental disconnection during patient movement or transport. The threaded design distributes connection forces evenly around the fitting perimeter, creating stronger seals than simple push-fit connections. Quality control testing ensures these connections maintain integrity under specified load conditions.
Some advanced urine bag systems incorporate quick-connect features that allow rapid bag changes while maintaining sterile conditions. These mechanisms include built-in disinfection ports and sealed transfer systems that prevent contamination during connection procedures.
Material Science Innovations in Drainage Bags
Advanced Polymer Engineering
Modern urine bag construction utilizes specialized polymers engineered specifically for medical applications requiring long-term fluid contact. These materials resist degradation from urine chemistry while maintaining flexibility and strength throughout extended use periods. Polymer selection considers factors such as chemical compatibility, biocompatibility, and environmental stress cracking resistance.
Cross-linking technology enhances polymer performance by creating molecular bonds that improve material strength and chemical resistance. This process results in drainage bags that maintain structural integrity even when exposed to aggressive cleaning agents or extreme temperature variations commonly encountered in healthcare environments.
Additive packages incorporated during polymer processing provide additional functionality such as UV resistance, antistatic properties, and improved clarity. These carefully selected additives enhance overall urine bag performance without compromising biocompatibility or sterility requirements.
Barrier Film Technology
Multi-layer barrier films used in premium drainage bags provide superior odor control and fluid containment compared to single-layer designs. These engineered films combine different polymer types to optimize specific performance characteristics such as oxygen permeability, moisture barrier properties, and mechanical strength.
Nano-layer technology enables the production of extremely thin barrier films that maintain excellent barrier properties while reducing overall bag thickness and weight. These ultra-thin films improve patient comfort by creating more flexible, less bulky drainage systems without sacrificing containment performance.
Coextruded barrier films integrate multiple functional layers during the manufacturing process, creating seamless transitions between different material properties. This manufacturing approach eliminates potential delamination issues while providing optimal barrier performance across the entire urine bag surface area.
Quality Control and Testing Protocols
Leak Testing Procedures
Rigorous leak testing protocols ensure that every urine bag meets stringent quality standards before reaching healthcare facilities. Pressure testing involves filling bags with test fluids and applying specified pressures for predetermined time periods. Any bags showing pressure loss or visible leakage are rejected from production batches.
Burst strength testing determines the maximum pressure each urine bag can withstand before failure. This testing establishes safety margins that prevent bag rupture during normal use conditions. Test results guide design improvements and material selection for enhanced product reliability.
Cyclic fatigue testing simulates long-term use conditions by repeatedly flexing and stressing bag materials. This testing identifies potential failure modes that might develop during extended drainage bag use, allowing manufacturers to address durability issues before product release.
Biocompatibility Verification
Comprehensive biocompatibility testing ensures that all urine bag materials are safe for prolonged contact with human tissue and body fluids. Cytotoxicity testing evaluates whether bag materials release harmful substances that could damage cells or tissues. These tests follow internationally recognized standards for medical device biocompatibility.
Sensitization testing determines whether repeated exposure to drainage bag materials could cause allergic reactions in sensitive individuals. This testing involves controlled animal studies that evaluate immune system responses to material extracts and direct contact exposure.
Irritation testing assesses the potential for bag materials to cause skin or tissue irritation during normal use. These evaluations consider both acute effects from short-term exposure and chronic effects from long-term contact with drainage bag components.
Clinical Implementation Best Practices
Proper Installation Techniques
Correct installation procedures are essential for ensuring optimal urine bag performance and preventing complications. Healthcare professionals must follow strict aseptic techniques when connecting drainage bags to catheter systems. Hand hygiene, sterile gloves, and proper disinfection of connection points prevent introduction of pathogens into the urinary system.
Positioning drainage bags below bladder level ensures proper gravity drainage while preventing backflow that could cause infections. The bag should hang freely without kinking the connecting tubing, which could impede drainage flow or create pressure buildup within the system.
Securing mechanisms must provide stable bag positioning while allowing for patient mobility and comfort. Adjustable straps and clips should be positioned to distribute weight evenly and prevent pulling forces on catheter connections that could cause discomfort or accidental disconnection.
Maintenance and Monitoring Protocols
Regular monitoring of urine bag function includes checking for signs of leakage, blockage, or contamination. Healthcare staff should inspect connection points, valve operation, and bag integrity during routine patient assessments. Early detection of problems prevents complications and ensures continued system effectiveness.
Output monitoring involves measuring and recording drainage volumes at specified intervals. This data helps healthcare providers assess patient hydration status and kidney function while identifying potential problems with the drainage system. Accurate documentation supports clinical decision-making and quality improvement initiatives.
Scheduled replacement intervals for drainage bags follow manufacturer recommendations and institutional policies based on infection control principles. Regular bag changes reduce contamination risks and ensure optimal system performance throughout the patient care period.
FAQ
How often should a urine bag be replaced to maintain hygiene?
Standard recommendations suggest replacing drainage bags every 5-7 days for long-term catheterized patients, though institutional policies may vary based on patient condition and infection control protocols. More frequent changes may be necessary if the bag becomes damaged, heavily soiled, or shows signs of contamination. Healthcare providers should always follow manufacturer guidelines and facility-specific procedures for optimal patient safety.
What materials make a urine bag leak-proof and safe for extended use?
High-quality drainage bags utilize medical-grade polyethylene or vinyl materials with multi-layer construction for superior leak resistance. These materials undergo extensive biocompatibility testing to ensure safety during prolonged contact with body fluids. Advanced manufacturing techniques include heat-sealed seams, reinforced connection points, and antimicrobial surface treatments that maintain bag integrity throughout the recommended use period.
Can urine bags be safely used during patient transport and mobility?
Modern drainage bags are specifically designed to accommodate patient mobility while maintaining secure, leak-free operation. Flexible mounting systems and reinforced connection interfaces allow bags to move with patients during transport or routine activities. However, proper positioning below bladder level must be maintained, and healthcare staff should secure the bag to prevent pulling on catheter connections during movement.
What signs indicate that a urine bag needs immediate replacement?
Immediate replacement is necessary when bags show visible cracks, leaks, or damage to connection points. Other concerning signs include cloudy or foul-smelling drainage that suggests infection, valve malfunction preventing proper drainage, or any compromise to the sterile system integrity. Healthcare providers should also replace bags if they become overfilled, as this increases infection risk and may cause system failure.

