Medical professionals require precision instruments that deliver consistent performance across diverse clinical environments. The reliability of medical devices directly impacts patient outcomes and procedural success rates. While feeding syringes serve critical functions in nutrition delivery, understanding the broader spectrum of medical instrumentation helps healthcare providers make informed decisions about equipment selection. Modern healthcare facilities depend on various specialized tools, including biopsy forceps, which exemplify the engineering excellence required in medical device manufacturing. These instruments must meet stringent quality standards while maintaining operational efficiency under demanding conditions.
Material Science and Construction Standards
Advanced Polymer Technologies
Medical-grade materials form the foundation of reliable feeding syringes and related instruments. Manufacturers utilize specialized polymers that resist chemical degradation while maintaining structural integrity during repeated sterilization cycles. The molecular composition of these materials determines their compatibility with various medications and nutritional solutions. Similar precision engineering principles apply to biopsy forceps, which require materials that withstand mechanical stress while maintaining sharp cutting edges. Advanced manufacturing processes ensure consistent material properties throughout production runs.
Quality control protocols verify material composition at multiple stages of production. Tensile strength testing confirms that components can withstand operational forces without failure. Chemical resistance evaluations ensure compatibility with disinfectants and sterilization agents commonly used in healthcare settings. These rigorous testing procedures apply across various medical instruments, including specialized devices like biopsy forceps that demand exceptional reliability. Material certification documentation provides traceability for regulatory compliance and quality assurance purposes.
Precision Manufacturing Processes
State-of-the-art manufacturing facilities employ computer-controlled machinery to achieve precise dimensional tolerances. Injection molding parameters are carefully calibrated to eliminate defects that could compromise instrument performance. Surface finish specifications ensure smooth operation and facilitate thorough cleaning between uses. The same attention to detail applies to manufacturing biopsy forceps, where precision machining creates sharp, durable cutting surfaces. Automated quality inspection systems detect variations that exceed acceptable limits.
Environmental controls within manufacturing areas prevent contamination during production. Clean room protocols maintain sterile conditions for components intended for single-use applications. Temperature and humidity monitoring ensures optimal curing conditions for polymer materials. Statistical process control methods track production variables to maintain consistent output quality. Regular calibration of manufacturing equipment guarantees dimensional accuracy across production batches.
Design Engineering for Clinical Performance
Ergonomic Optimization
Ergonomic design principles guide the development of medical instruments that reduce operator fatigue during extended procedures. Handle configurations are optimized for comfortable grip positions that minimize hand strain. Weight distribution analysis ensures balanced feel during manipulation tasks. Professional feedback from clinical users informs design iterations that improve usability. Similar ergonomic considerations apply to biopsy forceps, where precise control is essential for accurate tissue sampling procedures.
User interface elements are positioned for intuitive operation without compromising sterile technique protocols. Visual indicators provide clear feedback regarding instrument status and proper positioning. Tactile feedback mechanisms help operators confirm proper engagement and operation. Grip textures are engineered to maintain secure handling even when wearing protective gloves. Field testing validates ergonomic improvements under realistic clinical conditions.
Functional Integration Systems
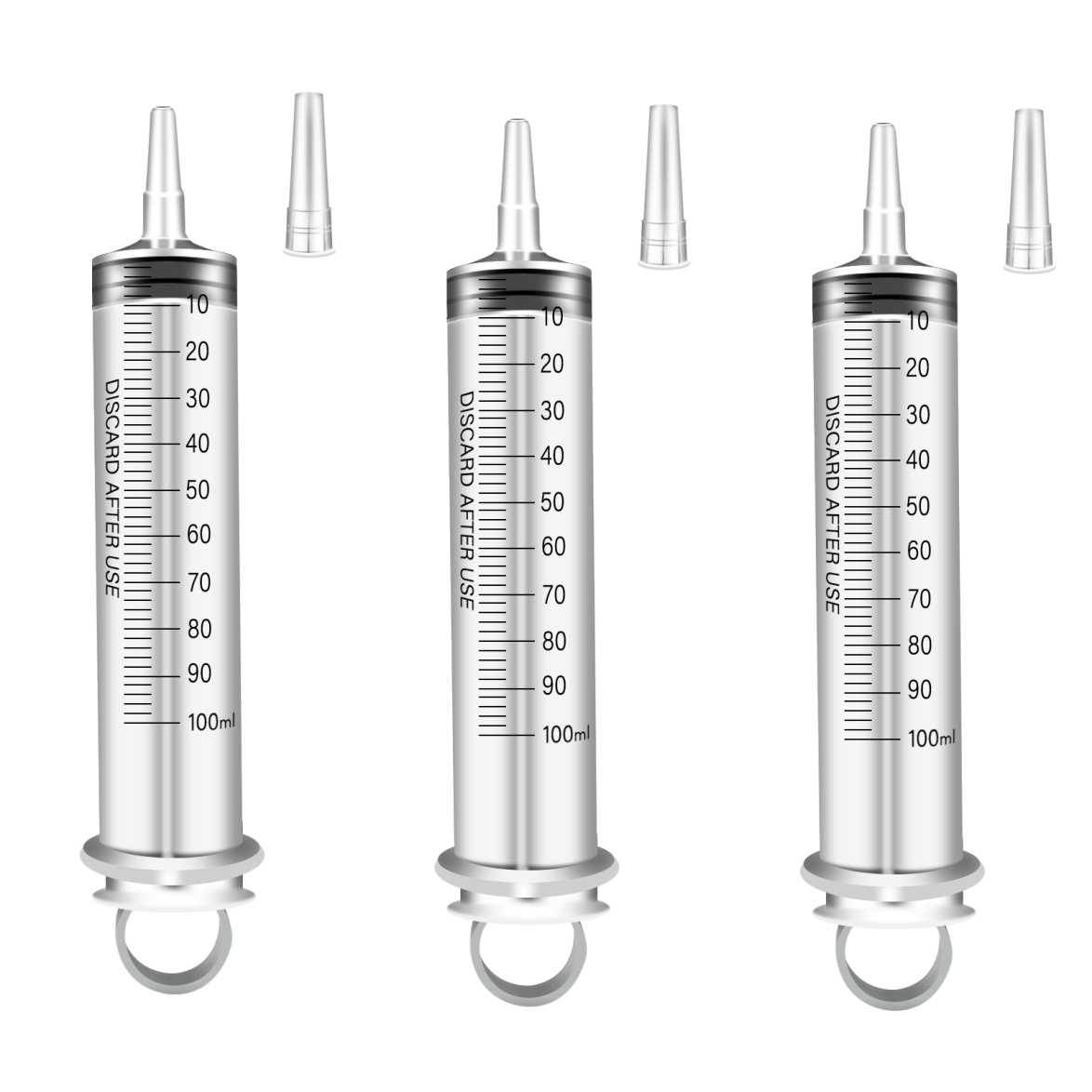
Modular design approaches enable compatibility with existing clinical equipment and workflow systems. Standardized connection interfaces facilitate integration with monitoring and delivery systems. Calibration markings provide accurate volume measurements for precise dosing applications. Electronic components, where applicable, are designed for electromagnetic compatibility with other medical devices. The integration principles extend to specialized instruments like biopsy forceps, which must interface seamlessly with endoscopic systems.
Safety mechanisms are incorporated to prevent accidental activation or misuse during clinical procedures. Locking mechanisms secure adjustable components in desired positions throughout use cycles. Pressure relief systems protect against over-pressurization in fluid delivery applications. Visual confirmation systems provide immediate feedback regarding proper instrument configuration. Redundant safety features ensure continued protection even if primary systems experience failures.
Quality Assurance and Validation Protocols
Comprehensive Testing Methodologies
Validation protocols encompass mechanical, chemical, and biological testing to ensure comprehensive device safety and efficacy. Fatigue testing simulates extended use cycles to identify potential failure modes before market release. Biocompatibility evaluations confirm material safety for patient contact applications. Environmental stress testing validates performance under extreme temperature and humidity conditions. The same rigorous testing standards apply to specialized instruments including biopsy forceps used in critical diagnostic procedures.
Sterilization validation confirms that recommended cleaning and sterilization protocols effectively eliminate microbial contamination. Residual chemical analysis verifies that sterilization agents do not leave harmful residues on device surfaces. Packaging integrity testing ensures that sterile barriers maintain effectiveness throughout product shelf life. Performance verification testing confirms that key functional parameters remain within specifications after sterilization cycles. Documentation systems track all testing results for regulatory submission and quality records.
Regulatory Compliance Framework
Medical device regulations require comprehensive documentation of design controls and manufacturing processes. Risk management procedures identify potential hazards and implement appropriate mitigation strategies. Clinical evaluation protocols demonstrate safety and effectiveness for intended use applications. Post-market surveillance systems monitor device performance and user feedback after commercial release. International standards compliance ensures global market access for medical instruments including biopsy forceps.
Change control procedures govern modifications to design specifications or manufacturing processes. Configuration management systems maintain version control for all device documentation and specifications. Supplier qualification programs ensure that component vendors meet required quality standards. Corrective and preventive action systems address quality issues and prevent recurrence. Regular management reviews assess quality system effectiveness and identify improvement opportunities.
Clinical Application Considerations
Procedural Efficiency Factors
Clinical workflow optimization requires instruments that integrate seamlessly into established procedural protocols. Setup time considerations influence device selection for high-volume applications. Single-use versus reusable options are evaluated based on cost-effectiveness and infection control requirements. Training requirements are minimized through intuitive design features that leverage existing clinical skills. The same efficiency principles apply to specialized instruments like biopsy forceps, where rapid deployment can be critical for patient outcomes.
Disposal considerations include environmental impact and waste management protocols for single-use devices. Storage requirements are optimized to minimize inventory space while ensuring product availability. Shelf life specifications allow for reasonable inventory turnover without waste concerns. Packaging design facilitates sterile presentation while minimizing packaging waste. Economic models compare total cost of ownership across different device options and usage patterns.
Safety and Risk Management
Patient safety protocols require comprehensive risk assessment for all medical device applications. Adverse event reporting systems track safety incidents and identify trends requiring corrective action. User training programs ensure proper technique and safety awareness among clinical staff. Emergency procedures are established for rare but serious complications associated with device use. Safety considerations are particularly critical for instruments like biopsy forceps, where improper use could result in patient injury.
Infection control measures prevent cross-contamination between patients and maintain sterile technique standards. Material compatibility evaluations ensure safe interaction with medications and biological fluids. Allergy considerations address potential reactions to device materials or components. Maintenance schedules for reusable devices ensure continued safety and performance throughout service life. Safety communication systems alert users to important safety information and device recalls when necessary.
Technology Evolution and Future Developments
Innovation Drivers in Medical Devices
Technological advancement continues to drive improvements in medical device design and functionality. Smart sensor integration provides real-time feedback regarding device performance and patient status. Miniaturization trends enable less invasive procedures with improved patient comfort. Advanced materials science develops new polymers with enhanced properties for specific medical applications. Innovation extends to specialized instruments like biopsy forceps, where improved cutting mechanisms enhance tissue sampling accuracy.
Digital connectivity enables remote monitoring and data collection for improved clinical outcomes. Artificial intelligence integration assists with procedure guidance and quality assurance. Sustainable design principles address environmental concerns while maintaining clinical performance standards. User interface improvements leverage modern human factors engineering to enhance usability. Predictive maintenance capabilities help prevent device failures before they impact patient care.
Market Trends and Adoption Patterns
Healthcare economics influence device selection criteria and adoption timelines for new technologies. Value-based care models emphasize outcomes over procedural volume, affecting device utilization patterns. Regulatory pathway evolution affects time-to-market for innovative medical devices. Global market expansion requires consideration of diverse regulatory and clinical practice environments. Market dynamics influence the development priorities for various medical instruments including biopsy forceps.
Clinical evidence requirements continue to evolve, demanding more comprehensive safety and efficacy data. Reimbursement policies affect the commercial viability of new medical technologies. Healthcare provider consolidation influences purchasing decisions and standardization efforts. Professional society guidelines shape clinical practice patterns and device utilization recommendations. Technology adoption cycles vary across different healthcare market segments and geographic regions.
FAQ
What factors determine the reliability of medical feeding syringes?
Reliability depends on material quality, manufacturing precision, and design validation through comprehensive testing. Medical-grade polymers must resist chemical degradation and maintain dimensional stability. Manufacturing processes require strict quality control to ensure consistent performance characteristics. Validation testing confirms device performance under simulated use conditions. The same reliability principles apply to other medical instruments like biopsy forceps, which require exceptional precision and durability.
How do regulatory requirements impact medical device design and manufacturing?
Regulatory frameworks establish mandatory safety and performance standards that guide design decisions from initial concept through commercial production. Risk management requirements influence material selection and safety feature implementation. Quality system regulations mandate comprehensive documentation and process controls. Clinical evaluation requirements demonstrate safety and effectiveness for intended applications. Compliance with international standards enables global market access for medical devices including specialized instruments like biopsy forceps.
What role does user feedback play in medical device development?
Clinical user input drives design improvements that enhance usability and safety in real-world applications. Ergonomic feedback helps optimize handle design and control placement for reduced operator fatigue. Procedural efficiency feedback identifies opportunities to streamline clinical workflows. Safety feedback highlights potential hazards that require design modifications or user training enhancements. Post-market surveillance incorporates ongoing user feedback to identify improvement opportunities and safety concerns for devices including biopsy forceps.
How do cost considerations affect medical device selection in healthcare facilities?
Healthcare facilities evaluate total cost of ownership including initial purchase price, maintenance costs, and operational expenses. Single-use versus reusable device decisions consider sterilization costs and infection control benefits. Volume purchasing agreements can reduce unit costs for high-usage devices. Clinical outcomes data helps justify higher-cost devices that improve patient safety or procedural efficiency. Economic models compare different device options including specialized instruments like biopsy forceps based on comprehensive cost-benefit analysis.

