Intravenous therapy represents one of the most critical delivery methods in modern healthcare, enabling direct administration of medications, fluids, and nutrients into a patient's bloodstream. The IV set serves as the essential conduit that makes this life-saving treatment possible, functioning as a sophisticated yet elegantly simple medical device that healthcare professionals rely on daily. Understanding how these systems operate provides valuable insight into their crucial role in patient care and treatment outcomes.
The complexity behind IV therapy delivery lies not in individual components but in how each element works together to ensure safe, controlled, and sterile fluid administration. From the initial fluid container to the final point of patient entry, every aspect of an IV set has been engineered to maintain precise flow rates while preventing contamination and ensuring patient safety throughout the treatment process.
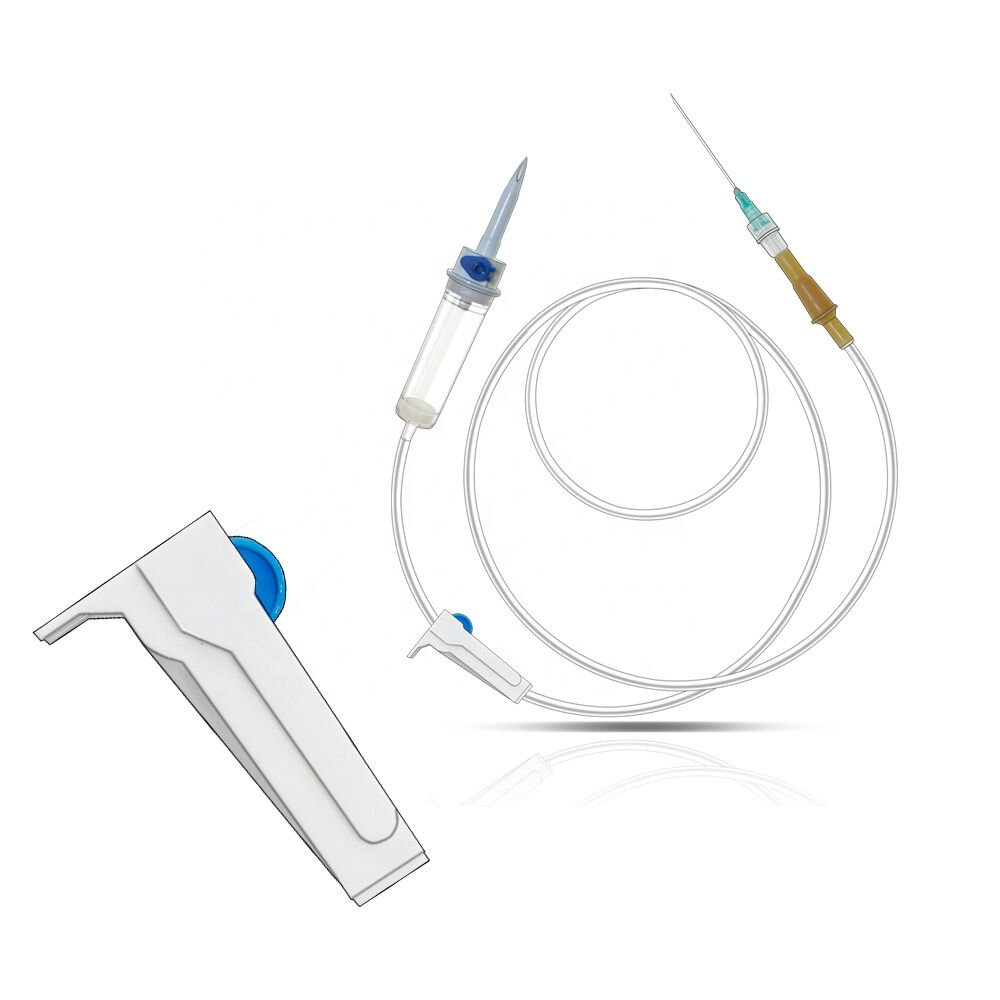
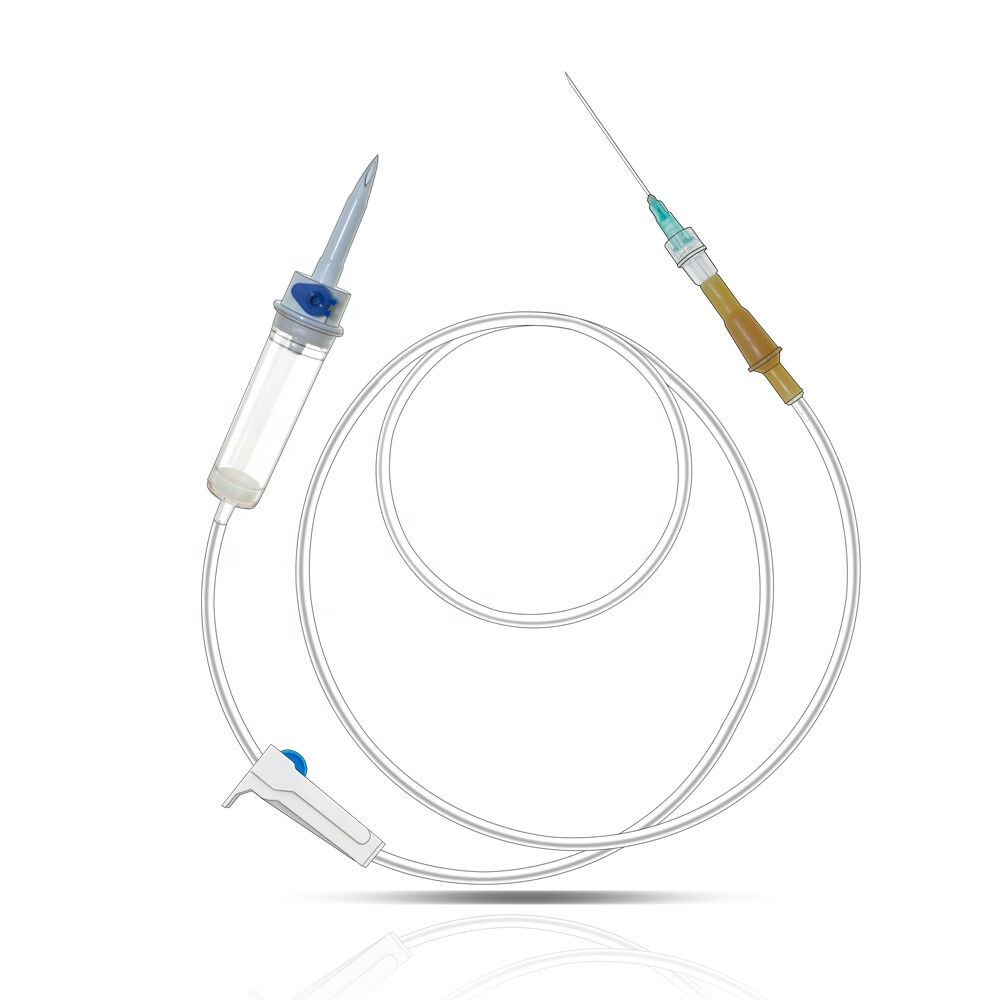
Essential Components of IV Administration Systems
Primary Tubing and Connection Points
The primary tubing forms the backbone of any IV set, constructed from medical-grade materials that maintain flexibility while resisting kinking and occlusion. This tubing connects the fluid source to the patient through a series of carefully designed connection points that ensure secure, leak-proof joints. The internal diameter of the tubing directly influences flow rates, with manufacturers precisely calibrating these dimensions to achieve predictable delivery patterns under various pressure conditions.
Connection integrity remains paramount throughout the entire system, as any breach could introduce contaminants or cause treatment interruption. Modern IV sets incorporate locking mechanisms and standardized connectors that prevent accidental disconnection while allowing healthcare providers to make necessary adjustments during treatment. These connection points undergo rigorous testing to ensure they maintain their seal under the mechanical stresses encountered during routine patient care.
Flow Control and Regulation Mechanisms
Flow control represents perhaps the most critical aspect of IV set functionality, determining how quickly medications and fluids reach the patient's bloodstream. Traditional roller clamps provide healthcare providers with manual control over flow rates, allowing precise adjustments based on patient needs and physician orders. These mechanical devices compress the tubing to varying degrees, creating controlled restrictions that govern fluid passage.
Advanced IV sets may incorporate additional flow regulation features such as inline filters, anti-reflux valves, and pressure-sensitive components that respond to changes in patient position or fluid container height. These sophisticated elements work together to maintain consistent delivery rates even when external conditions change, ensuring patients receive their prescribed treatments according to established protocols and safety guidelines.
Operational Mechanics and Fluid Dynamics
Gravity-Fed Delivery Systems
Most standard IV sets rely on gravitational force to drive fluid flow from elevated containers into patient veins, utilizing fundamental physics principles to achieve controlled drug delivery. The height differential between the fluid source and the patient creates hydrostatic pressure that overcomes venous pressure and pushes medications through the tubing system. This simple yet effective mechanism has proven reliable across decades of clinical use.
Healthcare providers must understand how gravitational systems respond to various factors including container height, patient position, and tubing configuration. Changes in any of these variables directly affect flow rates and delivery timing, requiring constant monitoring and adjustment to maintain therapeutic effectiveness. The predictable nature of gravity-fed systems makes them ideal for routine fluid replacement and medication administration where precise timing is less critical.
Drip Chamber Function and Monitoring
The drip chamber serves as both a flow indicator and air trap, allowing healthcare providers to visually monitor delivery rates while preventing air bubbles from entering the patient's circulatory system. This transparent chamber creates a controlled space where individual drops form and fall at measurable intervals, providing immediate feedback about system function and flow consistency.
Proper drip chamber operation requires maintaining an appropriate fluid level that covers the drip orifice while leaving sufficient air space for drop formation. Healthcare professionals use standardized drop factors to calculate precise flow rates, converting the visible drip pattern into accurate volume measurements. This visual monitoring system provides an essential safety check that helps detect blockages, air infiltration, or other complications before they affect patient care.
Safety Features and Contamination Prevention
Sterile Pathway Maintenance
Maintaining sterility throughout the entire fluid pathway represents a fundamental requirement for safe IV therapy, as any contamination could introduce dangerous pathogens directly into the patient's bloodstream. IV set manufacturers implement multiple safeguards including sterile packaging, closed system design, and materials that resist bacterial adhesion and growth.
The closed-loop design of modern IV sets minimizes exposure points where contaminants could enter the system, with sealed connections and sterile caps protecting unused ports. Healthcare providers follow strict protocols for maintaining sterility during setup and throughout treatment, including proper hand hygiene, sterile technique, and regular inspection of all system components for signs of compromise or contamination.
Air Embolism Prevention
Air bubble detection and removal systems built into IV sets provide critical protection against air embolism, a potentially life-threatening complication that occurs when air enters the circulatory system. The drip chamber acts as the primary air trap, allowing bubbles to rise and separate from the fluid stream before reaching the patient. Additional inline filters may capture smaller air particles that escape the primary chamber.
Healthcare providers must understand proper priming techniques that eliminate air from the entire system before connecting to patients. This process involves carefully filling all tubing segments while allowing trapped air to escape through designated vents or by temporarily opening downstream connections. Modern IV sets include design features that facilitate complete air removal while minimizing fluid waste and setup time.
Clinical Applications and Treatment Scenarios
Medication Administration Protocols
Different medications require specific delivery approaches that influence IV set selection and configuration, with factors such as drug compatibility, concentration limits, and infusion timing affecting system requirements. Healthcare providers must understand how various pharmaceutical formulations interact with tubing materials and whether special precautions are needed to maintain drug stability and effectiveness throughout the delivery process.
Continuous infusion protocols differ significantly from intermittent medication delivery, requiring IV sets with appropriate flow characteristics and connection options. Some treatments benefit from multi-lumen systems that allow simultaneous delivery of incompatible medications through separate pathways, while others require specialized tubing materials that resist drug absorption or degradation during extended contact periods.
Fluid Replacement and Electrolyte Balance
Fluid replacement therapy through IV sets plays a crucial role in maintaining patient hydration and electrolyte balance, particularly in critical care situations where oral intake is impossible or insufficient. The controlled delivery capabilities of IV systems allow healthcare providers to precisely manage fluid volumes and replacement rates based on individual patient needs and physiological responses.
Large-volume fluid administration requires IV sets capable of handling higher flow rates while maintaining system integrity and patient safety. Healthcare teams must monitor fluid balance carefully, adjusting delivery rates based on patient response, laboratory values, and clinical indicators. The reliability of IV set function becomes particularly important during extended treatment periods where consistent fluid delivery directly impacts patient outcomes.
Maintenance and Quality Assurance
System Monitoring and Troubleshooting
Effective IV set monitoring requires healthcare providers to regularly assess multiple system parameters including flow rate consistency, connection integrity, and patient response indicators. Visual inspection of the entire fluid pathway helps identify potential problems such as kinking, disconnection, or contamination before they compromise patient safety or treatment effectiveness.
Common troubleshooting scenarios include flow rate variations, air bubble accumulation, and connection leaks that require prompt attention and corrective action. Healthcare professionals must understand the underlying causes of these issues and appropriate response protocols that restore normal system function while maintaining patient safety. Documentation of system performance and any interventions provides valuable data for quality improvement initiatives.
Replacement and Disposal Protocols
IV set replacement schedules follow evidence-based guidelines that balance infection control requirements with practical considerations such as treatment duration and system performance. Most facilities implement standardized protocols that specify maximum use periods for different types of IV sets based on the fluids being administered and patient risk factors.
Proper disposal of used IV sets requires adherence to medical waste regulations and environmental safety protocols, as these devices may contain biological contaminants or pharmaceutical residues. Healthcare facilities must ensure staff understand appropriate disposal procedures and have access to designated collection systems that prevent exposure risks while meeting regulatory requirements for medical waste management.
FAQ
How long can an IV set remain in use before replacement?
Standard IV sets used for continuous infusion typically require replacement every 72 to 96 hours according to CDC guidelines, though this timeframe may vary based on the type of fluids being administered and institutional policies. Sets used for blood products or lipid emulsions generally need more frequent replacement, often every 24 hours, due to increased contamination risks and material compatibility concerns.
What causes air bubbles to form in IV tubing?
Air bubbles in IV tubing can result from several factors including incomplete system priming, loose connections that allow air infiltration, or rapid fluid administration that creates turbulence. Temperature changes and altitude variations may also cause dissolved gases to come out of solution and form visible bubbles within the tubing system.
Can IV sets be used for multiple different medications?
While IV sets can accommodate multiple medications through Y-ports or multiple access points, healthcare providers must ensure drug compatibility and follow proper flushing protocols between different medications. Some drugs require dedicated IV lines due to incompatibility issues, pH differences, or precipitation risks that could compromise patient safety or treatment effectiveness.
How do healthcare providers calculate proper IV flow rates?
IV flow rate calculations involve multiple factors including the prescribed volume, infusion duration, and the drop factor specific to the IV set being used. Healthcare providers use standardized formulas that convert physician orders into drops per minute or milliliters per hour, then adjust the flow control mechanism accordingly while monitoring actual delivery rates throughout treatment.